Sepsis
Sepsis is a rare life threatening condition that can develop rapidly from what might be otherwise innocuous infections. Working within Podiatry we are often presented with lesions on the lower limb and feet. With our appropriate training in wound care we are well placed in caring for your lesions and a recognising clinical signs of infection.
It is estimated that Sepsis affects 123,000 people in the UK each year, resulting in approximately 37,000 deaths. 70% of cases derived from an infection developed in the community. It is estimated that there is potential to reduce deaths by up to 10,000 per annum by early recognition of symptoms and optimising care.
How can Podiatrists help minimise the risk of developing Sepsis
As frontline Health Care Professionals we are best placed in the assessment and management of wounds to the lower limb and feet. We are also best placed to recognise the signs and symptoms of infection.
Localised invasive infection from a wound may develop into osteomyelitis within the bone or may lead to bacteria entering the bloodstream leading to cellulitis then sepsis if left untreated.
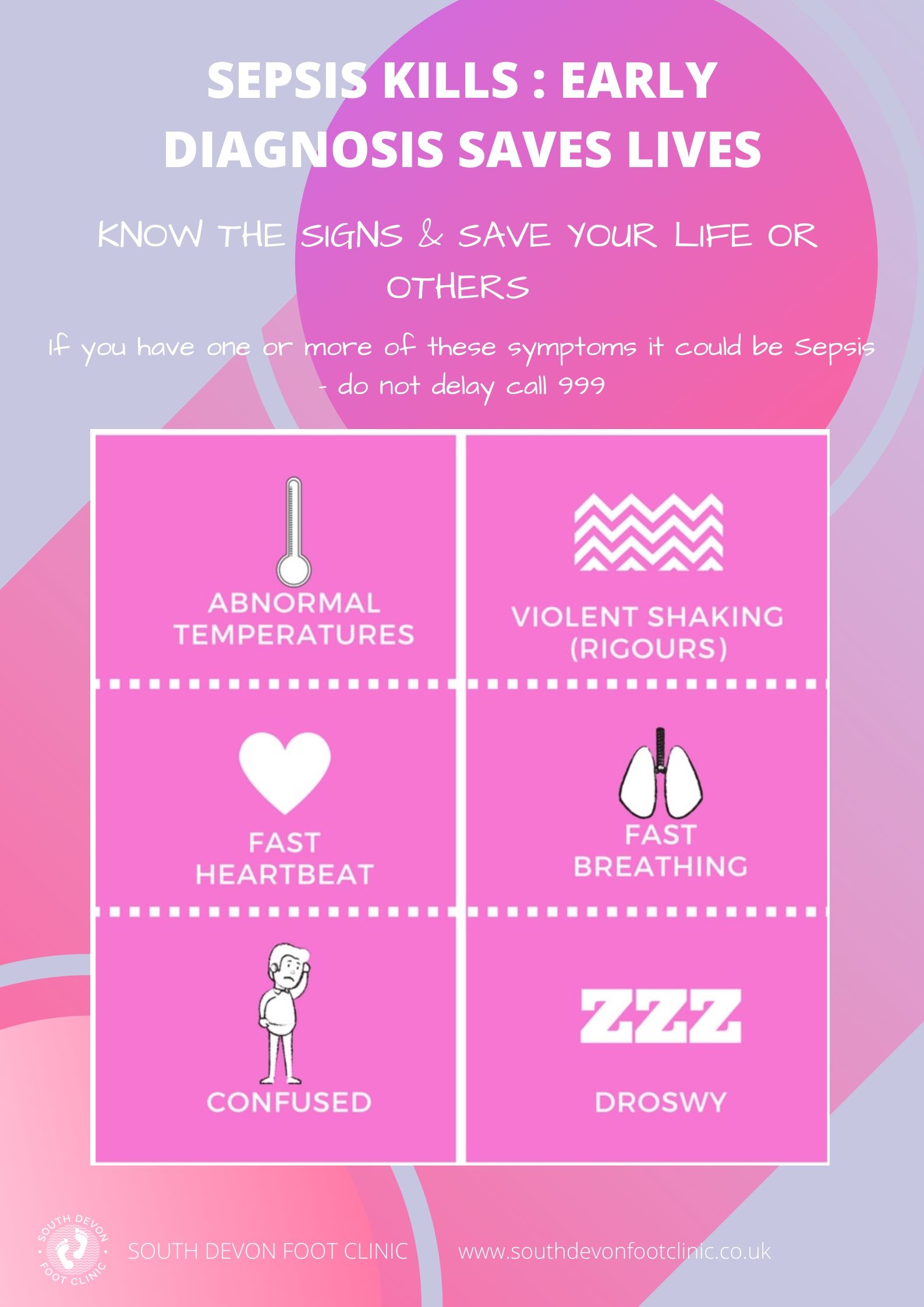
Sepsis is a time critical condition and should South Devon Foot Clinic suspect Sepsis during our assessment of your feet, the necessary steps shall be followed to ensure that you access prompt medical attention.
If you are a sufferer of Type 2 Diabetes Mellitus you may be at greater risk of developing Sepsis. There is a possibility that you may have a reduced immune response, neuropathy and pre-existing microvascular damage.
How is Sepsis treated?
In the case where we feel that you may have an infection but not symptoms of Sepsis, it may be recommended that you undergo a course of antibiotics and conservative management of the infection site. This recommendation will be communicated with your General Practitioner.
If you are too unwell to be treated at home or within an alternative setting, you will need to be omitted to hospital. Early recognition of Sepsis usually requires the use of antibiotics combined with a large amount of intravenous fluids. National Institute for Health and Care Excellence (NICE NG51, 2017) recommends that antibiotics should be administered within one hour of diagnosis.
The health care professionals within the hospital setting will take blood samples, provide you with intravenous fluids to rehydrate you, provide you with oxygen and examine where the infection has started.
People who are very ill or have gone into septic shock will need treatment from a critical care team. Some people may need surgery to remove infected tissue.
If the infection that caused your sepsis is starting to get better your healthcare team should let you know when it will be safe to go home.
Prevention is key
The following common conditions we see within Podiatry have the potential to develop into Sepsis. It is therefore recommended that you seek Podiatry assistance to manage them effectively.
- Ingrowing toe nails
- Lesions on diabetic feet
- Insect bites
- Cuts and blisters
- Foreign bodies within the tissue from walking barefoot
- Ulcerations